Understanding diabetes can seem complex, but the power of animation simplifies it beautifully. With the help of Alila Medical Media, a detailed video breaks down the differences between Type 1 and Type 2 diabetes, guiding you through the conditions in an engaging and easy-to-understand manner.
This video covers everything from the roles of glucose and insulin in the body to how these hormones behave differently in each type of diabetes. By the end, you’ll have a clear picture of how these chronic conditions develop, their symptoms, and methods of management.
Overview of Diabetes
Definition and Explanation
Diabetes refers to a group of conditions characterized by elevated levels of blood glucose, commonly known as blood sugar. When there’s too much glucose in your blood, it can cause a range of health troubles, some of which can be life-threatening. Diabetes can manifest in two major chronic forms: Type 1 and Type 2 diabetes. Additionally, there’s a temporary form called gestational diabetes that can occur during pregnancy and resolves typically after delivery. Pre-diabetes is a condition where blood glucose levels are higher than normal but not high enough to qualify as diabetes.
Impact on Health
The excessive glucose in your bloodstream can damage various organs and tissues over time. This can lead to complications such as heart disease, kidney failure, nerve damage, and even blindness. Managing blood sugar levels is essential to prevent these serious health issues and maintain overall well-being.
Statistics and Prevalence
Diabetes is a prevalent condition affecting millions of people globally. Type 2 diabetes is the most common, accounting for about 80-90% of all diabetes cases. The rising numbers are attributed to factors like sedentary lifestyles, unhealthy diets, and increasing obesity rates. Type 1 diabetes is less common and generally manifests at a younger age. It’s critical to address both types through effective management and education to curb this growing epidemic.
Introduction to Animation as a Learning Tool
Benefits of Using Animation for Medical Education
Animation offers a unique and engaging way to understand complex medical concepts. When you see dynamic, visual representations, it’s easier to grasp intricate topics like the workings of the human body. Animations can simplify complicated processes, making them more accessible to patients, students, and health professionals alike.
Effectiveness of Visual Learning
Watching animations taps into the power of visual learning. Visual aids have been proven to enhance memory retention and understanding. When concepts are illustrated, you can see how different parts of a system interact dynamically, which can be particularly useful for understanding diseases like diabetes and how they affect the body.
Engagement and Comprehension
Animations can make learning more engaging. Interactive visuals keep your attention and make the learning experience enjoyable. By seeing animations, you’re not just reading or listening; you are watching processes unfold in real-time, which has been shown to improve comprehension and recall.
Understanding Blood Sugar and its Role in the Body
The Process of Food Digestion
When you eat, your body begins breaking down the food into its fundamental components, such as carbohydrates, proteins, and fats. Carbohydrates are particularly important when it comes to understanding diabetes because they are the primary driver of blood glucose levels.
Breakdown of Carbohydrates into Glucose
Carbohydrates are broken down into glucose during digestion. This glucose is then absorbed into your bloodstream. Think of glucose as the fuel that your body’s cells need to function properly. Without it, your cells would not have the energy required to carry out their basic processes.
Glucose Transportation and Utilization
Once in your bloodstream, glucose needs to be transported to various organs and tissues to be used as energy or stored for later use. This transportation and usage process is heavily dependent on insulin, a hormone produced by the pancreas. Without proper insulin function, glucose remains in your blood, leading to high blood sugar levels.
Role of Insulin
Production by Beta Cells in the Pancreas
Insulin is produced by beta cells located within your pancreas. These cells release insulin into your bloodstream in response to rising glucose levels, such as after a meal. The release of insulin helps to manage and lower blood glucose levels.
Insulin Receptors on Target Cells
Insulin works by binding to receptors on the surface of target cells, such as muscle and liver cells. This binding allows these cells to take in glucose from the blood to either use it for immediate energy or store it for future use.
Glucose Intake and Storage
When insulin successfully binds to its receptors on target cells, those cells can absorb glucose. The liver plays a crucial role by storing glucose in the form of glycogen. Muscle cells use glucose for energy, especially during physical activity. If this absorption and utilization process is impaired, blood glucose levels remain high, which is the hallmark of diabetes.
Type 1 Diabetes
Causes and Risk Factors
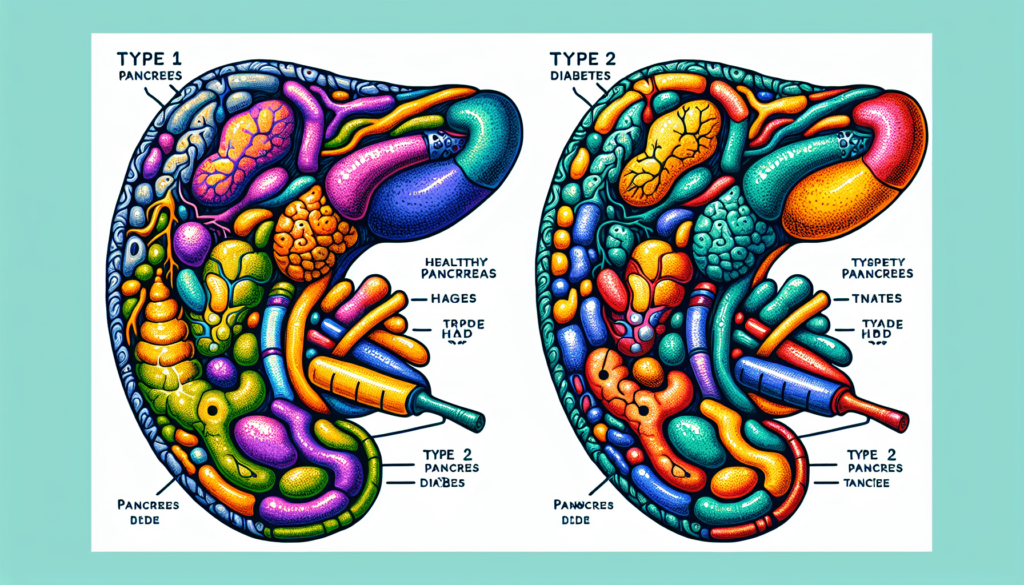
Type 1 diabetes is primarily caused by an autoimmune response where your immune system mistakenly attacks and destroys the beta cells in the pancreas that produce insulin. Although the exact cause is unknown, genetic factors play a significant role.
Pathophysiology
In Type 1 diabetes, the destruction of beta cells results in little or no insulin production. Without insulin, glucose cannot enter the cells and remains in the bloodstream, leading to elevated blood sugar levels.
Symptoms and Onset
Symptoms of Type 1 diabetes usually appear suddenly and are often noticed at a young age, before the age of 20. These symptoms include excessive thirst, frequent urination, unexplained weight loss, and fatigue.
Management and Treatment
Managing Type 1 diabetes typically requires insulin injections or the use of an insulin pump to regulate blood sugar levels. Additionally, patients need to regularly monitor their blood glucose levels and maintain a balanced diet to manage the condition effectively.
Type 2 Diabetes
Causes and Risk Factors
Type 2 diabetes is often associated with genetic factors, but lifestyle choices play a significant role as well. Obesity, inactivity, and unhealthy eating habits are major risk factors for this type of diabetes.
Pathophysiology
In Type 2 diabetes, the pancreas still produces insulin, but the body’s cells become resistant to its effects. This insulin resistance means glucose cannot efficiently enter the cells and remains in the bloodstream, leading to high blood sugar levels.
Symptoms and Onset
The symptoms of Type 2 diabetes develop gradually and typically appear after the age of 30. They include increased thirst and hunger, frequent urination, weight loss, fatigue, and blurred vision.
Management and Treatment
Management of Type 2 diabetes focuses on lifestyle modifications such as weight loss, increased physical activity, and a low-carb diet. Medications to improve insulin sensitivity and control blood sugar levels may also be prescribed.
Role of Lifestyle in Management
A healthy lifestyle is crucial in managing Type 2 diabetes. Regular exercise and a balanced diet can significantly lower blood sugar levels and improve insulin sensitivity, reducing the need for medications.
Comparing Type 1 and Type 2 Diabetes
Similarities and Differences
Both Type 1 and Type 2 diabetes involve issues with insulin and blood glucose management but differ in their causes and treatment methods. Type 1 is characterized by an absence of insulin due to an autoimmune response, while Type 2 involves insulin resistance.
Diagnosis and Testing
Both types of diabetes are diagnosed through blood tests that measure blood glucose levels. Common tests include the fasting plasma glucose test, the oral glucose tolerance test, and the A1C test, which provides an average blood glucose level over the past 2-3 months.
Implications for Long-term Health
Both types of diabetes, if not managed properly, can lead to long-term health complications such as cardiovascular disease, kidney failure, and nerve damage. Early diagnosis and effective management are vital to prevent these complications.
Prediabetes and Gestational Diabetes
Definition and Risk Factors
Prediabetes is a condition where blood glucose levels are higher than normal but not high enough to be classified as diabetes. Risk factors include obesity, sedentary lifestyle, and a family history of diabetes. Gestational diabetes occurs during pregnancy and increases the risk of developing Type 2 diabetes later in life.
Potential Outcomes
If not managed, prediabetes can progress to Type 2 diabetes. Gestational diabetes, although temporary, can also have long-term effects on both the mother and the child, including an increased risk of developing diabetes in the future.
Management Strategies
For prediabetes, lifestyle changes such as diet and exercise can prevent progression to Type 2 diabetes. Gestational diabetes management focuses on monitored blood sugar levels, a balanced diet, and regular physical activity to maintain health during pregnancy.
Innovative Solutions Through Animation
Case Studies and Examples
There have been numerous case studies showing the effectiveness of animation in healthcare education. For instance, animations illustrating how insulin works can help diabetic patients understand their condition better and adhere to their treatment plans more effectively.
Implementation in Healthcare Education
Healthcare professionals are increasingly using animations as part of patient education materials. These visual tools can help explain complex medical procedures, disease pathways, and treatment mechanisms in an easy-to-understand manner.
Feedback from Patients and Professionals
Both patients and healthcare professionals have reported positive feedback regarding the use of animations in medical education. Patients find them engaging and easier to understand, while professionals appreciate the enhanced communication and better patient compliance.
Conclusion
Summary of Key Points
Diabetes is a complex condition that significantly impacts health. Understanding the differences between Type 1 and Type 2 diabetes, and the role of lifestyle in managing the conditions, is crucial. Animation offers a powerful tool for educating patients and healthcare professionals alike.
The Future of Diabetes Education
The future of diabetes education looks promising with the increasing use of visual learning tools like animations. These tools can help simplify complex concepts, making them more accessible to everyone.
Encouraging Better Health Practices
By using innovative educational methods like animations, we can encourage better health practices and improve disease management. Understanding diabetes is the first step toward controlling it and leading a healthier life.







